Take Multiple Blood Pressure Readings for Lower BP

Blood pressure is a very controversial topic. Before you know it, they might say you should take medication when you actually don’t need it.
Apart from the usual “white coat hypertension”, the nervousness of coming to a doctor’s office causing a spike in your blood pressure, there appears to be something else wrong with taking the blood pressure reading only once.
Sure your doctor is very busy and it takes time to do the reading properly, but would you rather take medications for decades that you don’t need? I think everyone should insist that their blood pressure is taken accurately, and when doing it at home yourself it pays off to stick to the rules. Check out this article for in-depth information on how blood pressure should be taken: “Reading Blood Pressure: Do It Wrong and It Will Be Too High“.
Now what sticks out in that article are three things in my opinion that do not get enough attention, be it at the doctor’s office or in the user manual of your automated blood pressure monitor:
- the entire arm must be supported at heart level, for five minutes before you take the reading. How many times was this done properly, do you remember?

Please look carefully at the position of the arm. The entire arm is supported and at heart level (mid sternal level). This is much higher than what is stated in most blood pressure user manuals. The above is the correct arm placement, however. If you position your arm just a little lower, the blood pressure reading will be much higher and thus incorrect!
Source: Blood pressure measurement, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1120141/
2. you must wait 5-10 minutes or longer and relax.
3. you need to take the blood pressure up to 5 times in a row without a pause if the values are elevated, until you get a stable measurement.
Now this is really interesting. Consider a typical measurement:
152/91 here we get nervous obviously, but then ..:
135/91
131/85 (20 point drop!)
128/85 (repeated stable)
130/86 (normal measurement ‘noise’ +/- a few points)
Right arm (only one measurement):
131/84
Note that I did switch arms at the end for the final reading and the above measurements were taken in rapid succession, one after the other without a pause. As Dr. Batmanghelidj describes in his article, for some people, the first measurement is very high. A signal is sent to the brain to temporarily increase blood pressure because a blockage was detected. The blood pressure later normalizes; hence, after a couple measurements, the numbers stabilize to show your true blood pressure.
I have done the above experiment with two different blood pressure monitors, the second is a fairly expensive Omron product which I checked against a manual sphygmomanometer. The effect is always present, sometimes less dramatic, especially if the first reading is lower to begin with. For other people, however, usually the ones who have a normal range blood pressure reading in the beginning, the numbers remain about the same, despite repeated readings. This makes me believe that there may be an anatomical difference causing this effect in some people.
Is it reliable to measure 5 times in a row?
It appears when Dr. Batmanghelidj described his method, there was no scientific evidence back then but he knew from countless patients in his own experience that it is accurate. I have done some research to prove that taking many readings is not only accurate, it’s actually necessary for proper diagnosis of hypertension.
See:
Thirty-Minute Office Blood Pressure Monitoring in Primary Care
Quote: “OBP30 yields considerably lower blood pressure readings than OBP in all studied patient groups. OBP30 is a promising technique to reduce overtreatment of white-coat hypertension in primary health care.” What is OBP30? It’s a technique of repeating the BP measurements many times within 30 minutes: “OBP30 is performed with the patient sitting alone and undisturbed during 30 minutes while the blood pressure is measured automatically every 5 minutes, producing 7 readings. The resulting OBP30 is the mean of the last 6 blood pressure readings.”
Serial blood pressure measurements
In the above study they investigated and found that venous congestion does not have an effect on the BP accuracy. Some physicians believe that taking the BP too soon will lead to false low readings. This study confirms what I have been measuring, see example above, that’s why I switched arms and measured the right arm just once. I wanted to exclude the possibility of getting a false low reading on the left because of venous congestion due to having compressed the arm five times in succession.
Quote: “There was no increase in arterial blood pressure (ABP) oscillations when successive ABP readings were taken without an interval or even with venous congestion interposed. Contrary to the present belief, there seems to be no loss of reliability when blood pressure recordings are taken immediately one after another, in the clinical setting.“
Reading Blood Pressure: Do It Wrong and It Will Be Too High
Quote: “When the blood pressure cuff is tightened on your arm, the brain receives a signal. That signal, increase the blood pressure to compensate for the blockage. It is not until you pump up and release the blood pressure cuff 3 to 5 times that you will get an accurate reading. The difference in the first reading to the last could increased by 10 points or more.
Try It Yourself: If you have an automatic blood pressure cuff, take your blood pressure 5 times in a row. As soon as it deflates, re-inflate it. Write down the measurements each time. Note what the last three are. You will be surprised at the results.”
Prevalence of pseudoresistant hypertension due to inaccurate blood pressure measurement
In the above article they describe how measuring BP properly and repeatedly prevents 33% of patients to be wrongly diagnosed with hypertension.
The above article describes the phenomenon of how blood pressure rises abruptly when the cuff is inflated (‘reactive rise’).
Effect of anticipation and cuff inflation on blood pressure during self-measurement
In this article they call the ‘reactive rise’ phenomenon ‘pressor response’. Quote: “Our results support the existence of a pressor response during self-BP measurement that remains present after multiple BP readings.”
Principles and techniques of blood pressure measurement
In the above article they call it “cuff inflation hypertension”. Quote: “Cuff-inflation hypertension: Although in most patients the act of inflating a sphygmomanometer cuff does not itself change the blood pressure, as shown by intra-arterial62 and Finapres87 recordings, in occasional patients there may be a transient but substantial increase of up to 40 mm Hg coinciding with cuff inflation…”
Also they show in the illustration below why it is very critical to support the entire arm at heart level, compare the BP values below in A and B, and notice that in A the arm is at heart level, perpendicular to the torso:

Misleading measurements of blood pressure among the elderly
Quote: “…Cuff-inflation hypertension may also easily be confused with pseudohypertension and may even be considered in the differential diagnosis of of resistant hypertension if physicain is not aware of this entity. Cuff-inflation hypertension is induced by the excess and the rapid inflation of of cuff to a level far above the systolic blood pressure and by the muscular activity associated with the inflating cuff, while blood pressure is measured [2]. A neurogenic theory has also been postulated. It can be diagnosed by comparing the directly measured intraarterial diastolic pressure both before and after cuff inflation, and at the korotkoff phase V.”
Blood pressure difference between the measurements taken during cuff inflation and deflation
In the articles above there are references to wrist measuring devices. I happen to have two. The ‘reactive rise’ in blood pressure as seen by my measurements showed above does not occur in one of my wrist devices. The very peculiar thing about that device is that it measures BP while inflating, not deflating. So unlike upper arm devices, it doesn’t inflate the cuff quickly and then release slowly. It pumps up very slowly and then abruptly finishes and deflates. It appears the measurements taken with that device do not show a reactive rise or ‘cuff inflation hypertension’. I suspect it’s because there is no reaction taking place because there is no sudden blockage in blood flow. The article above shows some real data that might confirm what I have been seeing perhaps what Dr. Batmanghelidj meant in his description:
Quote: “…The manual SBP measured during cuff inflation was significantly lower by 4.3 mmHg (mean±SD: 110.6±9.7 vs 114.9±9.0) than that measured during cuff deflation…”
Quote: “This study showed that there is a transient reactive rise in IABP [invasive arterial blood pressure] values with NIBP [noninvasive BP] cuff inflation. … The exact mechanism for this effect is not known but may be attributed to the pain and discomfort from cuff inflation.”
The above study might be also describing the same phenomenon that was picked up by Dr. Batmanghelidj.
The above article has again support for the phenomenon that the first measurement is in general higher than subsequent measurements. Quote: “…the first sequential measurement was on average higher than the second, suggesting an order effect…Previous studies have shown that unilateral cuff inflation may increase SBP from 4 mm Hg to 9 mm Hg. Explanatory mechanisms include muscle compression, pain and discomfort during the measurement, and increased arousal as a result of the knowledge that BP is being measured.” Also they confirm the existence of a BP rise phenomenon when the cuff is inflated.
Body position and blood pressure measurement in patients with diabetes mellitus
This journal article also shows the different positions they used to measure blood pressure accurately. Note the bottom picture and how the entire arm is supported at heart level. Quote: “…the arm should be placed at right atrial level during all the BP measurements, regardless of the body position.”

My Recommendation
Remember this is not medical advice and I’m not a physician. However, if your BP reading is higher than what is considered desired, I would definitely insist on having the blood pressure taken properly, as described by Dr Batmanghelidj and many other physicians, which is also what the Merck Manual describes: the entire arm must be supported at heart level, you need to be relaxed for at least 5 minutes, back supported, feet on the ground, no talking, etc. If you are worried or stressed the reading will be much higher than your usual BP. If the arm is not correctly positioned for 5 minutes at heart level, it can lead to a reading 10-20 points higher.
What can go wrong when measuring blood pressure?
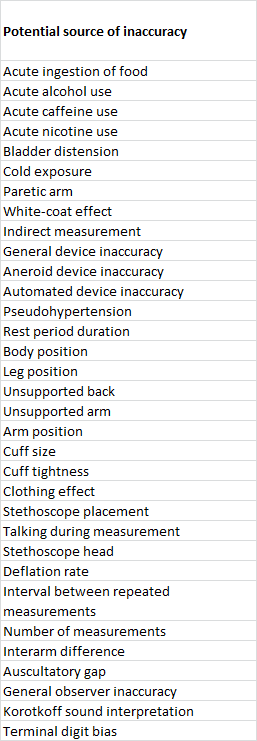
A lot can go wrong when you measure blood pressure incorrectly. See “Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review“. As far as I know, all errors result in higher blood pressure readings, except one: if you hold the arm above heart level. In real-life you will find that at least one or two errors in the list below were made, so you need to watch out, whether it’s at home or at the doctor’s office:
Interesting enough, the article mentions ‘interval between repeated measurements’. They cite two studies:

A great article which clears away a lot of confusion – thank you! I will now hold my arm at the correct level & wait 5 min. In the past I have taken consecutive readings with small time intervals between. e.g. Today – 148/88, 146/65, 140/80, 141/77, 137/80, 124/76, 128/74. PR: 64, 61, 58, 56, 57, 56, 55. I can be tensed up; PR indicates tension. I am 82
Hi Charles
thank you for your comments. At your age with those BP numbers, you have absolutely nothing to worry about. Those numbers would be good for 20 year old!
I agree the pulse rate indicates tension, i.e. when the pulse goes down (and often also BP) it often means the person is more relaxed than before.
If you see this happening often, simply wait a little longer (perhaps more than 5 minutes) before taking BP. It could simply be that the rest period was too short.
All the best, wishing you good health, and thanks again!
Savas
Thank you for such extensive research. I have been battling anxiety due to inaccurate BP readings. One doctor took my bp reading only once with me leaning forward with my arm dangling down and immediately prescribed me beta blockers. I refused to take them and now will follow your advise and update. Sincere thanks to you sir!!
you’re welcome. Please note that anxiety can briefly spike blood pressure well over 160 or 180 and is nothing to worry about as long as you have a detailed record of systematic home measurements.
Prescribing beta blockers after just one measurement doesn’t sound logical to me. I follow the number #1 rule of troubleshooting: before you try to fix something you need 100% evidence that something is really wrong, you need to know exactly what it is, and why/how the fix is going to help. In your case, the problem is likely not high BP, it’s high anxiety or stress levels, which are completely normal. Over 1/3 of the population has “white coat syndrome”, i.e. high BP only in the doctor’s office. Often it could also be called “doctors-don’t-care-to-measure-BP-correctly-because-insurance-always-pays-well” syndrome.
Savas
Thank you very much for the research
But why none of the health organizations offer your solution?
How can I be sure that your way is correct?
Hi XX
if you check my post one more time you will see lots of references. Some are made to the British Hypertension Society.
You will also want to take note of the fact that the leading health organizations today have no official authority. They are just instruments of the pharmaceutical industry, and so are universities to a degree as well. There is nothing that the pharmaceutical industry leaves to chance.
My post is about the ‘correct’ way to the measure blood pressure. Several cardiologists and nurses have confirmed that ‘this is indeed’ the correct method. However, the majority of practitioners doesn’t take the time or simply doesn’t care to do it right. Because any mistake they make increases your BP numbers, so they win. If it were the other way around you would see a very meticulous method being practiced.
Look for the “ABCs of Hypertension” from the 1980s or early 1990s, British Hypertension Society. See http://www.eoinobrien.org/wp-content/uploads/2008/08/A-B-C-of-Hypertension-Booklet-1981.pdf section Arm position and support
Hope this helps
Savas